Hospital A&E Safety: Behind the Headlines of a Damning Inspection Report at Medway Maritime
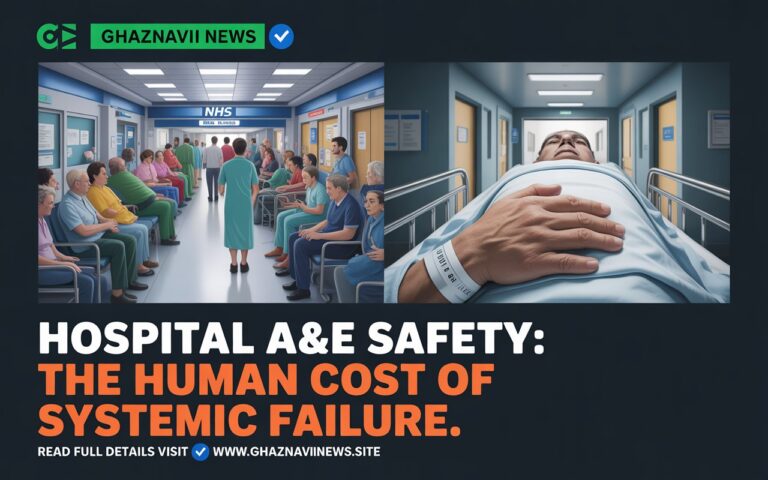
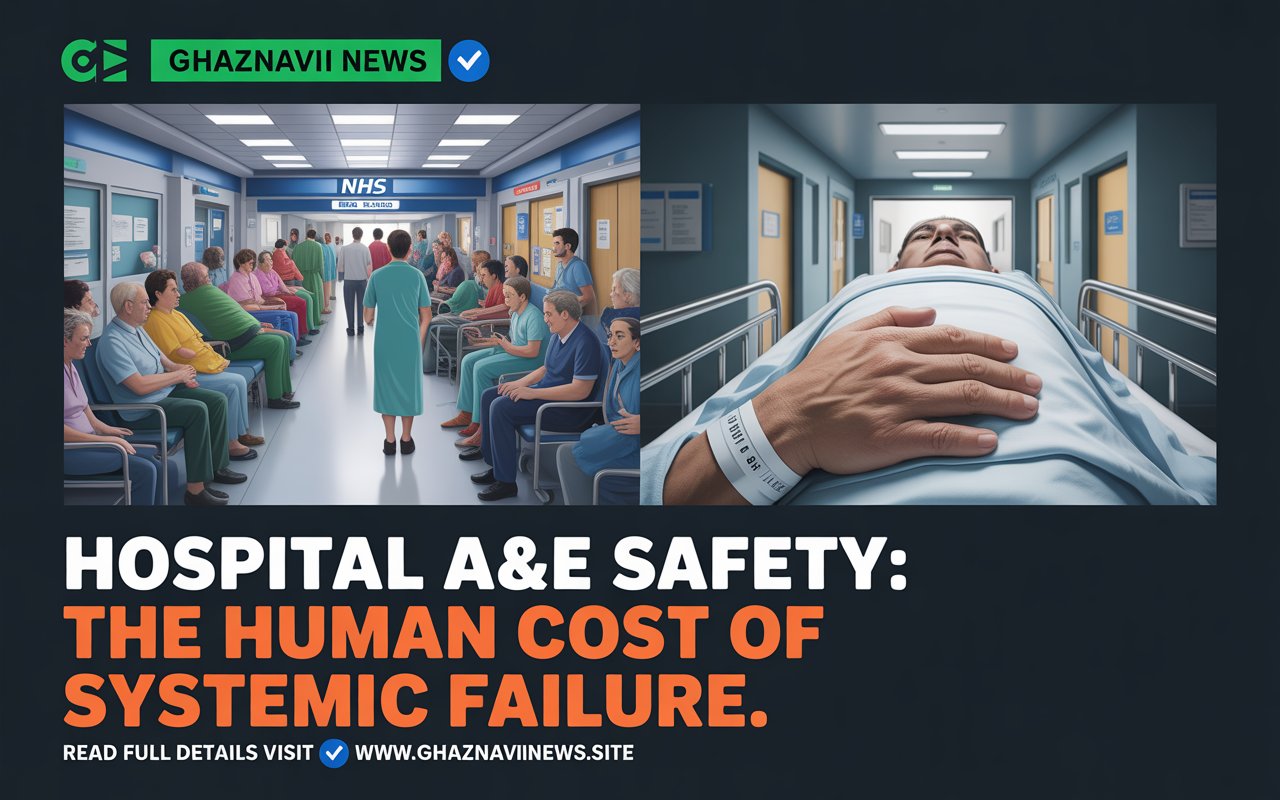
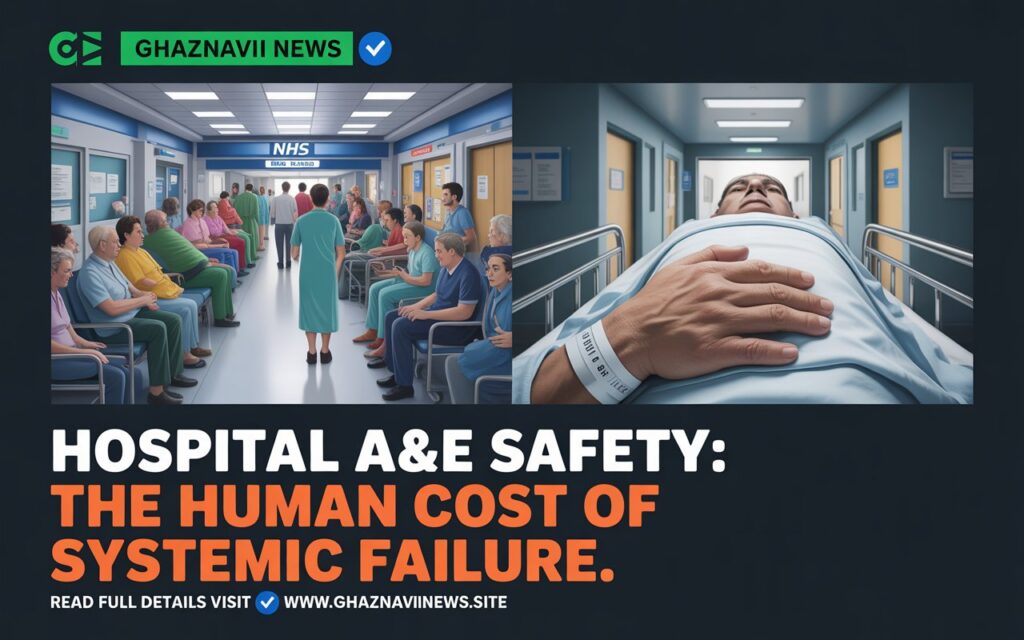
A hospital’s Emergency Department is more than just a medical facility; it is a barometer of a community’s healthcare system, a place where efficiency, compassion, and clinical excellence are tested under the most intense pressure. For the patients and staff at Medway Maritime Hospital in Gillingham, Kent, this pressure has become a constant, overwhelming reality. A recent unannounced inspection by the Care Quality Commission (CQC), the independent regulator of health and social care in England, has cast a stark light on the persistent challenges within its A&E department. While the report acknowledges some marginal progress, its core message is one of continued alarm: serious concerns about Hospital A&E safety, patient dignity, and the quality of care during busy periods remain fundamentally unresolved. This deep dive goes beyond the press releases to unpack the CQC’s findings, exploring what it truly means for a hospital to be deemed “inadequate” in safety, the real-world impact on patients, and the Herculean task facing an NHS trust struggling to keep its head above water.
The CQC’s Verdict: A Tale of Marginal Progress and Persistent Failure
The CQC’s report presents a complex and often contradictory picture. On the surface, there is a narrative of improvement. The overall rating for the emergency department was upgraded from “Inadequate” to “Requires Improvement.” The specific rating for the core question, “Is the service safe?” was also lifted from “Inadequate” to “Requires Improvement.” For the hospital’s leadership and communications team, these are the headlines they can point to as evidence of a turnaround.

However, this superficial progress masks a much grimmer underlying reality. The CQC found that the service was in breach of two fundamental legal regulations related to:
- Safe care and treatment.
- Dignity and respect.
This is not a minor administrative oversight. A breach of a legal regulation signifies a serious, systemic failure to meet the basic standards that patients have a right to expect. Furthermore, the CQC explicitly stated that concerns over how the service manages patient safety, dignity, and care during busy periods “remain ongoing.” This language indicates that the inspectors saw past the Trust’s action plans and identified a deep-seated, operational crisis that has not been solved.
The Human Cost: When “Requires Improvement” Means Patient Suffering
Regulatory ratings can feel abstract. The CQC report, however, grounds its assessment in the harrowing, first-hand experiences of patients, transforming bureaucratic language into a narrative of human distress.
The inspectors spoke with over 50 people during their visit. Some patients described their experience as “extremely unsatisfactory,” citing:
- Excessive noise levels creating a chaotic and stressful environment.
- Limited access to staff, leaving patients feeling ignored and vulnerable.
- Being cared for in inappropriate locations, such as corridors, which strips individuals of their privacy and basic dignity.
Perhaps the most clinically alarming finding was the failure in basic pain management. The report states that staff did not consistently record or reassess people’s pain levels. The consequence of this failure is not just a line in a report; it means that real people, in genuine distress, were left to suffer needlessly because their pain was not systematically tracked or addressed. This is a fundamental breach of the duty of care and a clear indicator of a system under such strain that it cannot perform its most basic functions reliably.
The Root Causes: A System Buckling Under Pressure
The CQC did not simply catalogue failures; it diagnosed the underlying causes. The problems at Medway Maritime are not the result of a few underperforming individuals, but of systemic issues that have crippled the department’s capacity to function.
The Staffing Crisis: A Department Running on Empty
At the heart of the Hospital A&E safety concerns is a critical shortage of skilled personnel. The inspectors found that the department lacks an adequate senior consultant cover and is missing national guidance on staffing levels.
This shortage creates a vicious cycle:
- High Patient Flow + Low Staffing = Overwhelmed Teams: As Roger James, the CQC’s Deputy Director of Operations in Kent and Medway, noted, they found “a very pressured service, with staff not always able to provide people with timely help, treatment, dignity, and respect.” Staff directly told inspectors this was due to “constant flow and capacity challenges.”
- Burnout and Low Morale: When staff are consistently unable to provide the level of care they were trained to give, it leads to moral injury, burnout, and high turnover, which further exacerbates the staffing shortage.
- Lack of Senior Oversight: Inadequate senior consultant cover means less experienced junior doctors are often making critical decisions without sufficient support, increasing the risk of clinical errors and compromising patient safety.
The Leadership Paradox: “Well-Led” But Failing?
In a curious contrast, the CQC rated the department as “Good” for being well-led. This seems to conflict with the damning findings elsewhere. How can a leadership be “good” while presiding over breaches of legal regulations and inadequate safety?
This rating likely reflects the CQC’s assessment that the Trust’s leadership recognizes the problems, has developed plans to address them, and is engaging with the regulator. Jonathan Wade, the Trust’s interim chief executive, openly admitted, “We try to ensure everyone feels safe in our care and has a positive experience but we recognise that despite the improvements recognised by the CQC, this is often not the case.” This honesty is commendable. However, the “well-led” rating raises a critical question: at what point does the ability to write an action plan become secondary to the ability to execute it and deliver tangible, consistent improvements on the frontline of care?
A Glimmer of Hope and The Long Road to Recovery
It is crucial to acknowledge where the department has succeeded. The report highlighted that the department performed well in handing over patients from ambulances, minimizing delays over 30 minutes and allowing ambulance crews to return to the community more quickly. This is a significant achievement that benefits the entire local emergency response network.
In response to the inspection, the hospital trust has apologized to patients and stated that it has recruited more doctors and nurses for the emergency department since the inspection. This is a necessary first step, but it is only a first step. Recruiting staff is one thing; integrating them into a functional, supportive, and sustainable system is another challenge entirely.
Conclusion: A Microcosm of a National Crisis
The situation at Medway Maritime is not an isolated incident. It is a potent microcosm of the pressures facing the NHS nationwide: soaring demand, chronic workforce shortages, and an estate often struggling to cope. The CQC report serves as a vital, public accountability mechanism, giving a voice to patients who have suffered and highlighting the heroic, yet overwhelmed, efforts of the staff.
Hospital A&E Safety
For the public, the report is a sobering reminder that Hospital A&E safety is not a given. It is a fragile state that requires adequate funding, strategic long-term workforce planning, and relentless operational focus. The upgrade from “Inadequate” to “Requires Improvement” is not a victory; it is a probationary notice. The real test for Medway Maritime NHS Foundation Trust is not whether it can satisfy the CQC on paper, but whether it can transform its emergency department into a place where every patient is guaranteed safe, timely, and dignified care—no matter how busy it gets.
What is the current CQC rating for Medway Maritime Hospital’s A&E?
The overall rating for the A&E department is “Requires Improvement.” Its safety rating was upgraded from “Inadequate” to “Requires Improvement,” but it was found to be in breach of two legal regulations concerning safe care and patient dignity.Hospital A&E Safety
What were the main safety concerns identified?
Key concerns included inconsistent pain management for patients, a shortage of senior consultants, patients being cared for in inappropriate locations like corridors, and a chaotic environment that limited staff access and compromised dignity.Hospital A&E Safety
Did the CQC report highlight any positive developments?
Yes. The department was rated “Good” for being well-led and was praised for its efficient handover of patients from ambulances, which helps get paramedics back on the road faster.
How has the hospital trust responded?
The Trust has apologized to patients and stated that it has recruited additional doctors and nurses for the A&E department since the inspection took place.
What does a breach of a “legal regulation” mean?
It means the hospital failed to meet a fundamental, legally enforceable standard set for all healthcare providers in England. In this case, the breaches were related to providing safe care and treatment and ensuring patient dignity and respect, which are among the most basic responsibilities of a hospital.Hospital A&E Safety
Table of Contents


Read More News